Can I use HRT if I have a family history of Uterine Fibroids?
What are uterine fibroids?
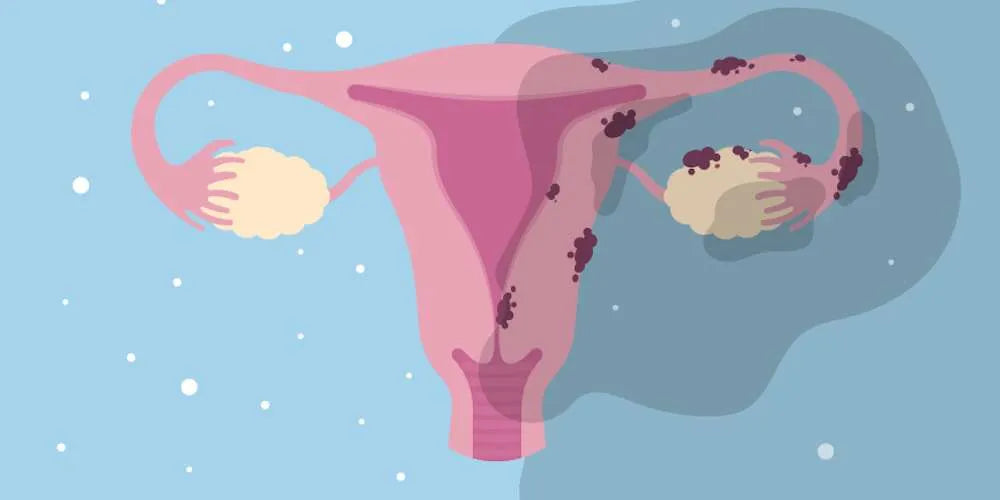
Uterine fibroids, or leiomyomas, are benign tumors in the uterus's muscular wall, common in childbearing women but possible at any age. Sizes range from tiny to large, and they can grow individually or in clusters.

Symptoms include heavy bleeding, long menstrual periods, pelvic pain, frequent urination, difficulty with bladder emptying, constipation, and back or leg pain.
While some women show no symptoms, fibroids can complicate fertility and pregnancy, potentially leading to cesarean sections, miscarriages, and preterm births. Their growth is linked to hormonal factors like estrogen and progesterone, particularly during reproductive years, and genetics may also increase risk.
Treatment varies from watchful waiting to medication and surgery, depending on symptom severity, fibroid size and location, age, and childbearing plans.
Are uterine fibroids common in women?
Uterine fibroids are common in women, particularly during reproductive years, with 70-80% developing them by age 50.
Not all women with fibroids experience symptoms or need treatment. Factors like age, race, family history, and lifestyle influence their prevalence and severity.
These benign tumors vary in size and are linked to hormonal levels of estrogen and progesterone, leading to symptoms such as heavy bleeding, pelvic pain, and sometimes fertility issues.
Risk is higher in African-American women, those with a family history, overweight individuals, and women who haven't given birth.

Regular gynecological check-ups are crucial for early detection and management, improving life quality and minimizing complications.
Are uterine fibroids dangerous?
Uterine fibroids are benign growths in the uterus that are not inherently dangerous but can cause symptoms and complications affecting quality of life and reproductive health.
Symptoms vary based on fibroid size, location, and number, including heavy menstrual bleeding leading to anemia, pelvic pain and pressure, urinary and bowel issues, and potential impacts on fertility and pregnancy, such as miscarriages or the need for a cesarean section.

Rarely, fibroids may lead to acute pain or are associated with leiomyosarcoma, a very rare cancer.
Many women experience mild or no symptoms, with fibroids often shrinking post-menopause due to decreased estrogen levels.
Treatment depends on symptom severity, fibroid characteristics, age, and pregnancy desires, ranging from watchful waiting to medication, procedures, or surgery.
Despite not being dangerous, fibroids can significantly affect well-being, highlighting the need for medical oversight and tailored treatment.
Does a family history increase the risk of fibroids?
Yes, having a family history of uterine fibroids increases the risk of developing them.
Women with first-degree relatives who have fibroids are at a higher risk, indicating a genetic component to fibroid development.
While the exact inheritance mechanism is unclear, genetic, and environmental factors together influence fibroid risk.

Known genetic mutations and chromosomal changes have been linked to fibroids, and ongoing research seeks to uncover more about their genetic basis.
Considering family history is crucial for early detection and management, especially for women at higher risk due to ethnicity, obesity, high blood pressure, or no history of pregnancy.
Discussing your family history with a healthcare provider is important for personalized monitoring and management of your reproductive health.
Can HRT cause fibroids to grow in postmenopausal women and cause health issues?
Yes, hormone replacement therpay can cause fibroids to grow in postmenopausal women and potentially lead to health issues.
Uterine fibroids are sensitive to estrogen, which can stimulate their growth. During the reproductive years, the natural fluctuations of estrogen and progesterone influence the development and size of fibroids. After menopause, the natural production of these hormones decreases significantly, which typically leads to a reduction in fibroid size and an alleviation of symptoms.

However, postmenopausal women who use estrogen supplementation, especially without adequate progesterone to balance its effects, may experience growth of existing fibroids or the development of new ones. This is because the supplemented estrogen can mimic the hormonal environment of the reproductive years, promoting fibroid growth.
The potential health issues related to fibroid growth in postmenopausal women on estrogen therapy include:
- Pelvic pain and pressure: As fibroids grow, they can cause discomfort, a sense of fullness or heaviness in the lower abdomen.
- Bleeding: Although less common in postmenopausal women, significant fibroid growth can lead to abnormal uterine bleeding.
- Urinary problems: Large fibroids can press on the bladder, leading to frequent urination or difficulty emptying the bladder completely.
- Impact on adjacent organs: Very large fibroids may press on other organs in the pelvis, causing a range of symptoms.
Given these risks, it's important for postmenopausal women considering alternative treatments for menopausal symptoms that do not involve estrogen to mitigate the risk of fibroid-related complications.
Safer Alternative Methods to HRT
If you have a family history of fibroids, caution is advised with Hormone Replacement Therapy (HRT). Estrogen and progesterone in HRT can elevate the risk uterine fibroids, as these hormones promote the growth of fibroids.
There are numerous non-hormonal methods and products available to manage menopausal symptoms, including nutritional supplements, vaginal moisturizers, and physical therapies.
NeuEve is hormone-free and is a safe natural product for relieving vaginal dryness. It has helped over 100,000 women to find relief from severe vaginal dryness, including those with the most severe type of vaginal dryness caused by pelvic radiation.
Disclaimer: This article is for information purposes only. It is about natural products, nutrients, and/or methods for managing discomforts associated with menopause or aging (not a true infection or disease). It is not medical advice for the treatment of any diseases.







Leave a comment