A Comprehensive Guide to Aerobic Vaginitis (AV)
What is Aerobic Vaginitis?
The term "aerobic" refers to a condition where life requires the presence of air or free oxygen. An example of this is aerobic exercise.
Aerobic exercise, also known as cardiovascular exercise, is designed to increase your heart rate. During aerobic exercise, your blood circulates rapidly throughout your body, and your lungs take in more oxygen.
 Aerobic exercise
Aerobic exercise
It's important to note that aerobic vaginitis (AV) is not related to aerobic exercise. AV is a specific type of vaginal dysbiosis that occurs when aerobic bacteria, which thrive in the presence of oxygen, overpopulate the vagina.
This is distinct from bacterial vaginosis (BV), which is caused by anaerobic bacteria that do not thrive in oxygen-rich environments, like fish that cannot survive outside of water. AV, on the other hand, is caused by aerobic bacteria that can grow in the presence of air, like animals that live on land but not in water. Additionally, facultative bacteria, which can thrive in both aquatic and terrestrial environments, are also associated with AV, much like ducks.
Symptoms of AV can include vaginal itching, burning, unusual discharge, and discomfort.
AV was first described by the Belgium OB/GYN doctor Dr. Donders in 2002. It is characterized by a decrease in vaginal lactobacillus and the presence of predominantly aerobic bacteria.
The aerobic bacteria may come from four possible sources: fecal contamination, skin, bladder, and the intimate partner. Common causative bacteria include E. coli, Enterococcus, Group B streptococcus, Klebsiella, and Staphylococcus.
Aerobic vaginitis treatment
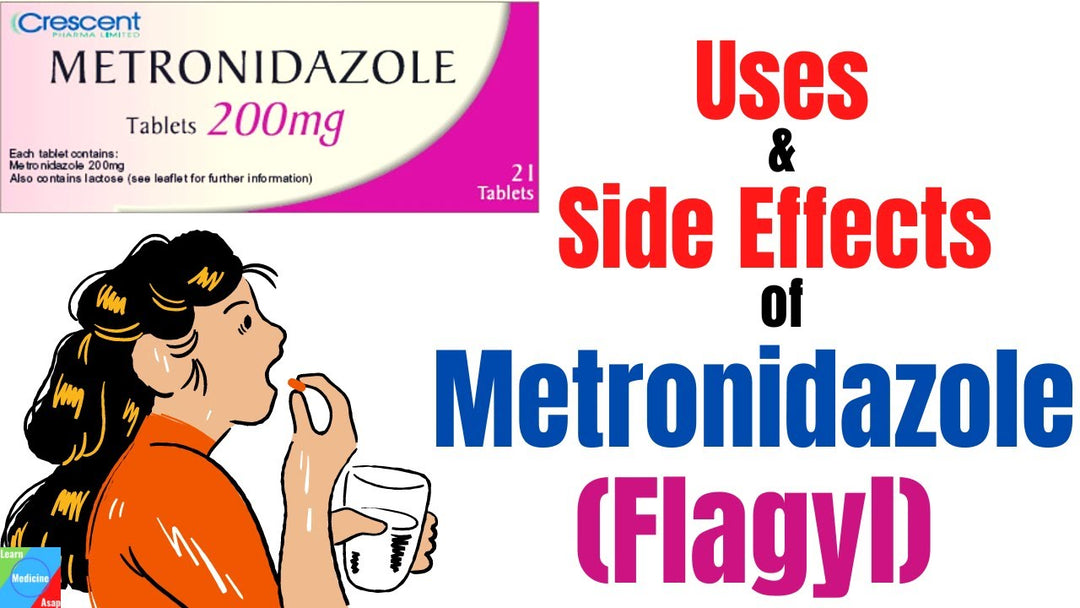
Aerobic vaginitis are often treated with antibiotics,including clindamycin, kanamycin, and fluoroquinolones. But antibiotics often fail to clear AV. Due to lack of effectiveness, drug-resistant bacteria or yeast infections are a common outcome. Because AV can be caused by multiple different bacteria, there has been no single antibiotic effective against all AV cases.
Boric acid has not been effective. Repeated use often causes more severe inflammation due its irritation to the sensitive tissue. As a well-known pesticide, long-term use of boric acid may result in infertility and other negative consequences.
Many products for clearing BV are available on the market. But there has been none for AV.
We've created the first self-care product for AV, called AV Clear (previouslly AV NIL). We put it through rigorous testing and improvments to make sure it works well.

The product is offered on our website and also on Amazon. Each pack has 3 suppositories. Like other NeuEve products, AV Clear is made with all-natural and food-grade ingredients. It can clear AV-associated discomforts safely without side effects.

A recent survey involving 18 volunteers with varying severities of AV asked five questions about their symptoms: very severe, severe, moderate, slight, and no symptoms, both before and after using AV Clear. Their responses were presented in a bar chart, and Chi-square analysis showed highly significant recovery.
This product has helped over 1,000 women worldwide find relief from AV, including some doctors with stubborn cases that antibiotics failed to resolve. They experienced relief after using AV Clear.
Unlike other products, such as boric acid, which kill all bacteria nonselectively, NeuEve relieves AV by balancing the microbiome. It suppresses only harmful bacteria while supporting beneficial bacteria.
If you're curious about how AV Clear works, you can read about it in this article:
How does NeuEve kill bad bacteria without harming good ones?
After AV is cleared, we recommend taking probiotic supplement. Restoring the balance of the vaginal microflora after antibiotic treatment is crucial to prevent recurrence and maintain vaginal health.
How can I prevent aerobic vaginitis?
After AV bacteria are cleared, their previous parking spaces become open. Any bacteria can come and take the vacated spaces. If good bacteria come, you are recovered. But if bad bacteria come, you may develop a new dysbiosis. This can be either AV or BV, depending on what bacteria take the vacated places.
Therefore, it is important to do a maintenance after you use AV Clear to make sure only good bacteria will come and take the vacated places.
Below are the recommended procedures.
1. Select the right maintenance product
The recommended maintenance is based on your age and health condition.
If you are healthy, the maintenance products are:
- NeuEve BV Clear, age under 40
- NeuEve Gold, age 40-50
- NeuEve Silver, age 50-55
- NeuEve Silk, age over 55.
If you have a health condition listed below:
- breastfeeding
- birth control (pills or patches)
- hormonal IUD
- hysterectomy
- cancer therapy
- lichen sclerosus
- Sjogren's syndrome
- polycystic ovary syndrome (PCOS)
- endometriosis
- medications like antidepressants, antihypertensives, and/or antiallergics
The maintenance products are:
- NeuEve Gold, age under 40
- NeuEve Silver, age 40-50
- NeuEve Silk, age over 50
2. The maintenance procedure
- Choose a suitable maintenance product that fits your age and health condition.
- On the next day after your last AV NIL application, you may start the maintenance product. If it is BV Clear or Gold, use it once a week. Silver, once every 5 days. Silk, twice a week.
- If your lab test shows a good number of protective Lactobacillus (>70%), you do not need to take probiotics. Otherwise, you can take probiotics. This article provides more details about how to use probiotics.
- You can take oral probiotics daily. But for a vaginal Lactobacillus insert, like V-Probiotics, you can use it between the applications of maintenance suppositories. For example, if you use BV Clear or Gold on Mondays, you may use a V-Probiotics insert daily from Tuesdays to Sundays.
- We recommend that you do at least 3 months of maintenance. If you can remain symptoms free for 3 months, you may be symptoms free for a long time.
Reduce Bacterial Load in Reservoirs
After your AV is cleared, AV bacteria in the vagina are eliminated, but a small number of AV bacteria might have escaped and hide in other places not reached by AV NIL. These places are called "reservoirs."
There are 4 possible reservoirs that may harbor AV bacteria to re-infect the vaginal tract after the initial clearance.
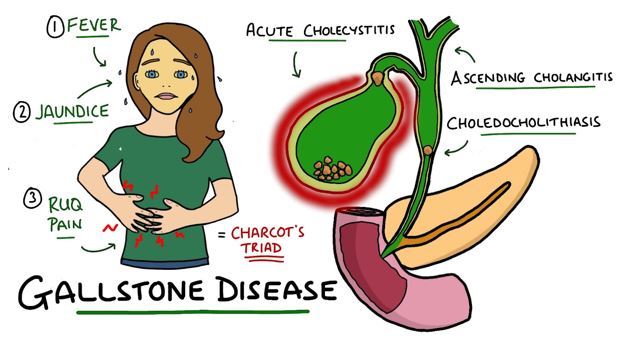
- The bladder, which often harbors E. coli, Enterococcus, etc.
- The colon, which often harbors E. coli, Enterococcus, group B streptococcus, etc.
- The skin, which often harbors Staphylococcus, etc.
- The intimate partner, who may harbor AV bacteria from you and give them back to you later.
1. Reduce bacterial load in the bladder
Summer is the season to have more frequent UTIs.
Hot weather can lead to increased sweating, which can, in turn, reduce the volume of urine in your bladder. When you don't urinate frequently enough to flush out the bladder, it can create an environment where bacteria can thrive. This bacterial overgrowth can potentially lead to frequent UTIs. Additionally, some of these bacteria may migrate to the vagina, increasing the risk of AV.
Hence, maintaining proper hydration, particularly during the summer months, is crucial for the well-being of both the bladder and the vagina.
You may take supplements and drink a lot of water described in this article to reduce bladder bacterial load:
Dietary supplements for managing recurrent UTIs (https://help.neueve.com/kb/dietary-supplements/dietary-supplements-for-preventing-recurrent-utis)
2. Reduce unwanted bacteria in the colon
Fecal matter consists of numerous bacterial species, but only a select few have the potential to cause AV (Aerobic Vaginitis) in the vagina. To minimize the presence of undesirable bacteria in the colon, consider incorporating probiotic supplements into your routine and increasing your consumption of probiotic-rich foods such as yogurt, kefir, kimchee, and sauerkraut (opt for pickled sauerkraut, not canned). This supplement Yeast Reset designed for reducing the Candida yeast may also help reduce unwanted AV bacteria, like E. coil and Staphylococcus, in the gut.

In addition, you can make lifestyle adjustments to reduce the risk of fecal contamination:
- Switch to 100% cotton underwear and change it at least once a day.
- When wiping, always go from front to back to decrease the likelihood of fecal contamination.
- Clean the anal area with mild soap at least once daily.
3. Reduce unwanted bacteria on the skin
The skin is not a sterile surface; it hosts millions of bacteria, with Staphylococcus being the most common among them. If your vaginal microbiome lab report indicates the presence of this bacterium, it could likely originate from your skin.
 To reduce Staphylococcus on the skin, the best method is to wash the skin with a gentile soap.
To reduce Staphylococcus on the skin, the best method is to wash the skin with a gentile soap.
4) Reduce unwanted bacteria in the partner
If an AV case is associated with group B Streptococcus, your partner may be a carrier. Even if he doesn't display noticeable symptoms, research has shown that spouses of women infected with group B Streptococcus can test positive for the same type of bacteria in their urine. Therefore, men can potentially be a source of for various AV-associated bacteria.
If you've had sexual intercourse and AV reoccurs, your partner could potentially be a source of the bacteria. It's important to note that men do not develop AV themselves, so any AV-related bacteria in men may be temporary. During your AV treatment, it's advisable to abstain from sexual activity for at least two weeks. It's also a good idea for your partner to maintain good hygiene by using soap and staying well-hydrated to help flush the bladder with strong urine pressure. This way, once your AV is cleared, your partner will also have a reduced risk of carrying the bacteria.
However, if your spouse has painful urination, it is an indication that he may have UTI and need to be treated by doctor.
5) Boost immune resistance Clearing bacteria from all potential reservoirs can be challenging. An alternative approach is to enhance the vaginal immune resistance. Using NeuEve products can assist in boosting vaginal immune resistance.
After successfully clearing AV, premenopausal individuals can consider a three-month maintenance regimen. If you are under 40 years old, you can use NeuEve BV Clear; if you are between the ages of 40 and 50, NeuEve Gold is suitable. This maintenance involves using one suppository per week and skipping the week during your menstrual period. If you remain AV-free for three months, you may enjoy long-term relief from AV.
However, for peri or postmenopausal individuals, vaginal atrophy is a common cause of AV. In the presence of vaginal atrophy, the vaginal lining becomes thin and lacks the normal exfoliation process, which is akin to dandruff shedding from the scalp. As a result, harmful bacteria like E. coli can adhere to the vaginal lining for longer periods. It's important to manage vaginal atrophy to promote vaginal health and reduce the risk of AV recurrence. If you are between the ages of 50 and 55, you can use NeuEve Silver once every 5 days or Silk (>55) twice a week for maintenance.


Attached bacteria are removed by cell exfoliation.
After AV is cleared, it may come back to cause recurrence. The reason is that the cause of AV, vaginal atrophy, is still there. If you reverse vaginal atrophy, the normal skin surface cell exfoliation will resume and attached bacteria will be removed regularly. AV may not come back
Therefore, for postmenopausal women to stop AV from coming back, the key is to relieve vaginal atrophy.
This article explains why maintenance is important.
NeuEve Silk (age >55), Silver (50-55), and Gold (<50) can help reverse vaginal atrophy. If you start with a lower phase like Silk, you can move up a phase after 1-4 months. You should reach the highest phase Gold for the best result to clear and stop bacterial growth. After using NeuEve suppositories for a few months, the atrophied lining skin becomes thicker, and vaginal cell exfoliation resumes. This increases the resistance of the vaginal lining skin. AV may not come back.
How long do I need to do the maintenance for vaginal atrophy relief? This depends on how long you you wish to remain sexually active. If you want to keep your sex life for 20 more years, you will need to keep the maintenance for 20 more years. The reason is that vaginal atrophy is not a disease that can be cured. It is an aging outcome, like wrinkles. If you stop applying cream on the face, wrinkles will show up. Likewise, if you stop applying NeuEve, vaginal dryness will return and you may have painful sex again. Dysbiosis like AV may come back. The NeuEve Gold is the longest-lasting product as you only need to use it once a week.

NeuEve Gold for vaginal atrophy
However, if you are not sexually active after AV is cleared, you can use NeuEve Gold for 1 month and use the NeuEve Balm Cream for continuous maintenance. One jar lasts 3-4 months.
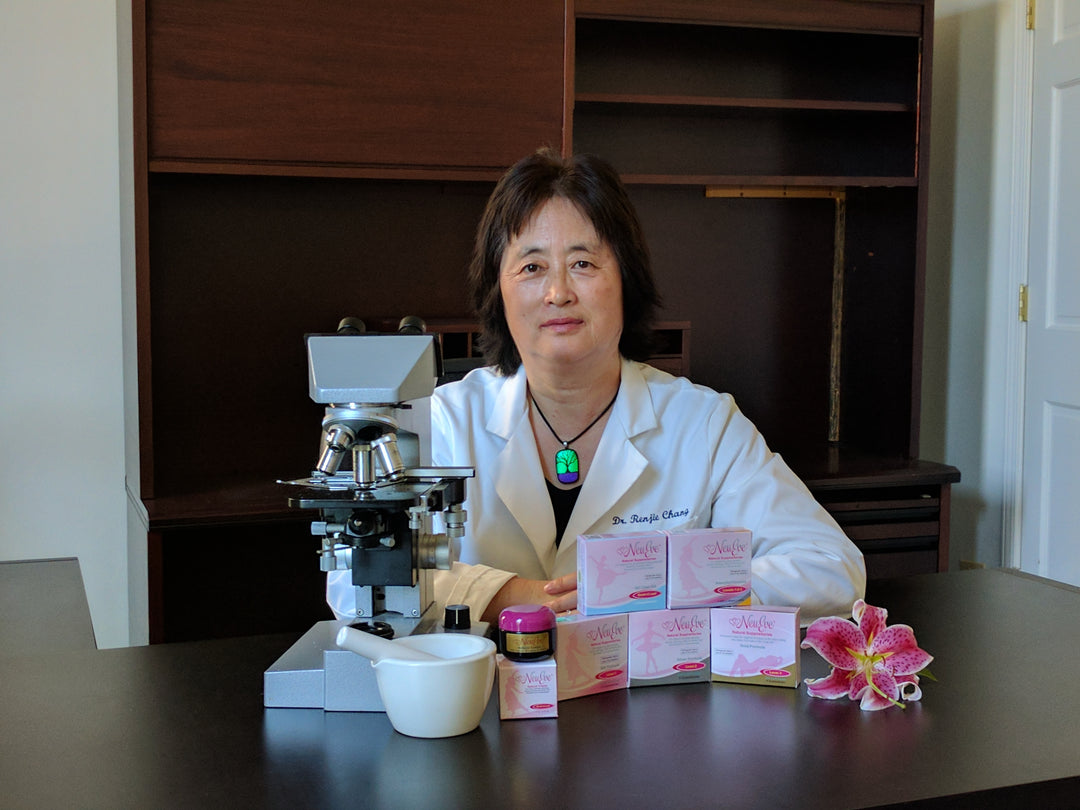
Meeting Dr. Donders
In 2019, Dr. Chang visited Dr. Donders in Europe. They discussed recent advancements in AV management.

FAQ:
What are the differences between AV and BV
Aerobic vaginitis (AV) and bacterial vaginosis (BV) are two distinct vaginal conditions, each characterized by different microbial imbalances in the vaginal ecosystem. Here are the differences between the two:
Microbial Imbalance:
• Bacterial Vaginosis (BV): BV is characterized by an overgrowth of anaerobic bacteria in the vagina, like Gardnerella vaginalis, Prevotella spp., and others. Lactobacilli, the beneficial bacteria, are decreased in BV.
• Aerobic Vaginitis (AV): AV, on the other hand, is associated with an overgrowth of aerobic or facultative bacteria, like Escherichia coli, Staphylococcus spp., Streptococcus spp., Klebsiella, and Enterococcus spp. In AV, the levels of lactobacilli are also reduced, but the microbial composition is distinct from BV.
Symptoms:
• Bacterial Vaginosis (BV): BV is often characterized by a thin, grayish-white vaginal discharge with a fishy odor, especially after sexual intercourse. Some women with BV may experience itching or burning sensations.
• Aerobic Vaginitis (AV): AV can present with symptoms such as itching, redness, burning, pain, redness, and an increase in vaginal discharge, but no apparent fishy odor. The discharge in AV is typically yellowish or greenish in color and may be more viscous than the discharge associated with BV.
Similarities Between AV and BV
Both AV and BV have an increase in vaginal pH, which becomes less acidic and decreased the presence of vaginal Lactobacillus species.
Both have similar risk factors including sexual activity, multiple sexual partners, and douching. They are not considered a sexually transmitted infection (STI), but may increase the risk of STIs.
Both have similar complications, such as an increased risk of negative pregnancy outcomes and pelvic inflammatory disease (PID).
How is AV diagnosed?
If you have been treated for yeast or BV, but did not find relief, your condition may not be yeast or BV. Your vaginitis may be AV. For a clear diagnosis, it is important to do a lab test.
Vaginal microbiome test can detect AV. The following labs can do a vaginal microbiome test. The vaginal microbiome test may cost about $150 per test. It is expensive but you may ask them if their test is covered by your medical insurance, Medicare, Medicaid, or HSA/FSA account.
The Juno lab has offered our NeuEve customers a group discount. If your lab test shows aerobic or facultative bacteria, like Escherichia coli, Staphylococcus spp., Streptococcus spp., Klebsiella, and/or Enterococcus spp., you may have AV.
Is vulvodynia related to AV?
Vulvodynia is a condition characterized by chronic pain or discomfort of the vulva with an unknown cause. The pain can manifest as burning, stinging, itching, or rawness.
However, with the advent of vaginal microbiome testing using cutting-edge Next-Generation Sequencing (NGS) technology, many cases previously diagnosed as vulvodynia have been identified as Aerobic Vaginitis (AV), associated with E. coli, Enterococcus, Streptococcus, Staphylococcus, and/or Klebsiella. To a lesser degree, some cases of vulvodynia have been associated with yeast infections.
Are recurrent UTIs related to AV?
Urinary tract infections (UTIs) are highly prevalent among women, and recurrent UTIs or recurrent cystitis (RC) pose significant challenges in postmenopausal women. Due to their proximity, bacteria colonizing the vagina can easily migrate into the urinary tract.
A new study using vaginal microbiome analysis has discovered that the vagina can act as a reservoir for enteric bacteria, and aerobic vaginitis (AV)—characterized by a reduction in Lactobacilli and an increase in enteric bacteria such as E. coli—can lead to recurrent UTIs.
Current guidelines recommend antibacterial prophylaxis for women with recurrent UTIs. However, frequent and prolonged use of antimicrobial agents can lead to intractable cystitis.
Therefore, a non-antibiotic method that can naturally clear AV may offer a safer and more effective solution for recurrent UTIs.
Is Lactobacillus iners related to AV?
However, there is one exception to note: Lactobacillus iners is a bad apple in the family of Lactobacillus. It is often associated with an increased risk of vaginal dysbiosis. If you see the presence of L. iners in your lab test and you also have discomforts like BV, but BV care products did provide relief, you may have a special type of L. iners-related AV. L. iners secretes a cytolytic toxin called inerolysin that lyses (kills) your vaginal lining skin cells and may cause burning and discharge.
Lactobacillus iners-associated dysbiosis presents a unique challenge. Lactobacillus iners, within the Lactobacillus family, has a tendency to cause dysbiosis by releasing a cytolytic toxin known as inerolysin. This bacterium is facultative and gram-positive. Neither BV or CV care products are equipped to provide relief in such cases. However, AV-NIL has shown promise in providing relief, possibly due to the bacterium's facultative nature, making its dysbiosis resemble that of Aerobic Vaginitis (AV).
L. iners-related dysbiosis is a relatively new condition and may not be widely recognized in the medical community. This is why many doctors might be unfamiliar with it. However, we have developed the first self-care product for relieving AV and L. iners-related cases. To date, hundreds of women with AV and L. iners-related dysbiosis worldwide have used AV NIL and found relief.

Disclaimer: This article is for information purposes only. It is about natural products, nutrients, and/or methods for managing vaginal odor or microbial imbalance-related minor discomforts (not a real disease). It is not medical advice for the treatment of any diseases.
*************************************************************************************
Product review for AV NIL
Emily, August, 2023
Worth it!
I had AV for 3.5 years. I got it after breastfeeding when my estrogen was low. It took 2 years and many doctors telling me there was “nothing wrong” to get the proper diagnosis. And even then I had to ask to be tested for it! Don’t give up! It took me 5 rounds of AV-nil success. I had a very stubborn case. And after the fifth round, I still felt “off” down there until I had used vaginal probiotics for a few nights. I know from previous testing that I had almost no protective bacteria! All that to say - if you’re on the fence - it’s worth it! The NeuEve team responds quickly if you need help or if it doesn’t work the first time for you. If you’re reading this review, you’ve been to many appointments already, and this is less than the cost you will pay there. I’m now using oral and vaginal probiotics and feel much better. And gold for maintenance. Your life can and will get better! There is hope!
Helped me clear cytolytic vaginosis (CV)
Anonymous, August, 2023
Alicia, August, 2023
I did 3 boxes of AV NIL recently followed by Gold for the BV. My AV bacteria was gone at the next testing and my good bacteria was significantly higher. I did also take a oral probiotic.

After AV NIL. I continued Gold after this for another two boxes to get rid of the last bit of Gardnerella. I went from 39% good bacteria to 95%.
Sam, July 2023
AV NIL
I have tried so many other products and this was the only one that helped me.
Thank you for making this product. If you are a woman struggling with AV it’s the product for you.
Sol, March 2023
I have Strep B. It’s Aerobic, and I started using AV NIL first week of March. I can say my life is back. I am very thankful. Now, I will be maintaining the Gold . More blessings.
FINALLY RELIEF
I started using silver after treating my AV with the AV-NIL treatment protocol. I am finally symptom free and feel like I am beginning to truly heal. I am so thankful to have found a safe hormone free product that truly works for me. I look forward to a better quality of life. Thank you NeuEve!
Heather, December 2022
I was diagnosed with AV in June. I took three rounds of antibiotics with no success. Then in August I was diagnosed with lichen planus (probably from the antibiotics). I’m not really responding to the steroids either and still have the AV.
I have finally cleared my Enterococcus faecalis after months of treatments with no results. My last PCR test confirming Enterococcus faecalis was at the end of September. At the time I had just started using the Silver. When I heard about the Av-nil trial, I decided to give it a try. I Started with a half suppository each night, but went down to 1/3 of the last suppository for the remaining nights due to exterior irritation. I have followed up with the gold each week after, used as a 1/2 suppository. I had my PCR test redone, and sure enough, I am all clear. No bacteria aerobic or anaerobic of any kind. Finally!








Hello , I took antibiotics for
What we thought was a urinary track infection-
Then several rounds of fluconazole for yeast infection -
Have had severe abdominal / pelvic pressure for 3 months …. no discharge …. Burning ….. and intermittent backache .
A month ago I began using vaginal estrogen cream due to dryness .
Do you offer products to help ?
Thank you
I need this 😩
I am a postmenopausal widow with vagina atrophy and now seeing a p floor therapist. Have itching and burning and full feeling..urine test neg then vaginal swab which showed e.coli. Tried an antibiotic but 4 pills in caused liver pain so quit. Am now on 2 biofilm disruptors, oregano oil and Interphase plus, and vagibiom suppositories to add more lactobacillus. Wanting to try your products as it sounds like AV. I want to start without the microbiome test first as I know I have e.coli and have already added the lacto b. Do you recommend buying just one kit first? Do I add the Silk now or wait until a.coli has killed off? I do not want to do antibiotic # 2 choice…
Hi! I have recurrent av, clindamycin helps but the av keeps getting back. Last time i was tested there were both aerobic bacterias and lactobacillis. I don’t know exact bacterias but probably e coli since i also have recurrent uti’s. I am 36 yrs old, i also have lichen
schlerosus and possibly endometriosis. Do you have recommendations which product would be best? Can i use your products while trying to get pregnant?
I have aerobic vaginitis caused by 5 rounds of antibiotics I had to take to get rid of endometritis. I have been burning on and off for 3 -4 months. I just took ampicillin 500 mg 4x a day for one week and no improvement. Do you think your company can help me?
Leave a comment